Health & Wellness
Beat Generation
Three decades after the first artificial heart transplant, little progress has been made in building a man-made ticker that lasts. Hopkins’ researchers aim to change that.
There’s a modest paper sign slapped on a basement door in The Johns Hopkins Hospital’s gleaming Sheikh Zayed Tower that alerts all passers-by: “New Artificial Heart Being Developed Behind These Doors.”
Knock on the door, and Jacopo Biasetti, a bearded 31-year-old postdoctoral student from San Remo, Italy, will likely answer. The room, about the size of a storage closet, holds a table, and, as of early fall, about a dozen tall cylinders of argon and nitrogen gas, remnants from the days when the room served as, well, a storage closet. On a table, there’s a high-speed, high-sensitivity video camera—resembling the size and shape of a small toaster—focused on a vial of plasma and hooked up to a computer. The boxy camera, a bunch of optical filters, and the vial rest on a polished stainless-steel stand that Biasetti and a Ph.D. student fabricated to hold and focus the contraption. It may not look like much, but the device allows him to observe on the computer screen a key blood protein interacting with platelets and other blood-related phenomenon in real time, which researchers have “lit up” with a special fluorescent material in unprecedented, high-definition detail.
“Right now, we have the capabilities to do something that no other group is able to do,” he says in a thick Italian accent, “even though we are in a small room with gas tanks.”
Welcome to the humble yet promising beginnings of the Johns Hopkins Heart Initiative, a 10-year, $100 million-plus program to build the world’s first permanent, totally artificial heart. The multidisciplinary effort involves researchers from across Hopkins’ schools of medicine, engineering, and its Applied Physics Laboratory, all concentrating on a single goal: “It’s our Manhattan Project, our lunar landing project,” says Dr. Duke Cameron, Hopkins’ chief of cardiac surgery and the man behind the idea. “It’s the same kind of model.”
If it seems as if we’ve already cracked this nut, we haven’t. Not by a long shot.

A traditional artificial heart, the kind Hopkins’ docs hope to render irrelevant.
More than 30 years ago, Dr. William DeVries implanted the world’s first artificial heart in a Seattle dentist named Barney Clark, who lived for 112 days on the device, known as the Jarvik 7. Since then, scientists have cloned sheep, invented the Internet, and perfected liposuction, but they still haven’t created an artificial heart that will keep someone alive for more than several months. Currently, only one totally artificial heart is approved by the federal government for use in patients, but it has proven to be effective for only up to 18 months.
So what’s the holdup?
To get an idea of what researchers are up against, try this little exercise: Do a pushup. Now two. Now keep at it for an hour or two. Tough, eh? Your heart essentially does the same thing all day and all night—35 million times a year-—for your entire life. How would you ever power such a thing? Battery technology has come a long way in recent years, but not that long a way.
Now think about how your heart speeds up when you stand up, or share a kiss, or watch a scary movie. How do you tell a mechanical heart to do the same? None of the current crop of artificial hearts or prototypes possess a true brain-heart connection.
Enter Duke Cameron. At 63 years old, he’s the old man of the cardiology department, a renowned specialist in surgically repairing problems with the aorta. In the middle of our interview in his office, he gets a text, excuses himself, and, like Superman, changes out of his shirt and tie into blue hospital scrubs, runs down to the OR, and bolts back 10 minutes later. He also manages to travel to places like Cuba, Egypt, and Saudi Arabia to perform life-saving heart surgeries free of charge on kids and adults. In other words, he’s the kind of guy you’d want opening up your chest.
“He probably asks Questions that nobody had ever thought of.”
Cameron says the idea for the heart initiative came to him from DeVries himself, who visited Hopkins in 2007 to give a talk. After the program, the two surgeons started chatting and Cameron asked him why he thought there hadn’t been significant progress in artificial heart technology. “He said to me—tongue-in-cheek—‘I guess we haven’t had the right people working on this project.’ I took it to mean that this was an opportunity for Hopkins.”
Cameron batted around the idea with colleagues for the next several years, and when he became chief of cardiac surgery in 2010, he made it one of his goals. DeVries came back to campus in February 2014 to officially kick things off.
“We’ve had mechanical hearts for 30 years, but they all have significant liabilities, limitations to how long they can be in place,” says Cameron’s colleague Gordon Tomaselli, chief of cardiology, who has been involved with the project from its start. “What we need is a paradigm-shifting change in technology. We thought this would be an opportunity to bring the best and brightest that Hopkins has from medicine, engineering, and the Applied Physics Lab to attack the problem.”
“Essentially, we’re crowdsourcing it to some of the smartest people in the world,” Cameron says.
In fall of 2013 , as part of his efforts to drum up support, Cameron hosted an educational and exploratory meeting at Hopkins’ Homewood campus. In the room were a dozen researchers from the schools of medicine and engineering. He gave a 10-minute talk about heart failure, and spoke of how hundreds of thousands of people are diagnosed annually with conditions that would benefit from new hearts, but because of a shortage of viable organs, only 2,000 to 2,500 transplants take place each year. (More than 4,200 patients, most suffering from end-stage heart failure, are currently on the national heart-transplant waiting list.) He spoke about Barney Clark, the current state of artificial hearts, and what the challenges were. Then he took questions.
An engineer by the name of Joe Katz spoke up first. “So, if we’re going to design a replacement heart, does it have to be in the center of your chest or can it be many places around the body?”
Huh? The doctors glanced at each other around the room.
“What I mean is, can it be several pumps, distributed around the body, working together, like you’d find on an airplane?”
“I was blown away,” says Cameron. “I thought to myself, ‘Thousands of people have worked on this problem, but I wonder if Joe was the first to ask that question.’ I thought, ‘This is a guy we’re really going to enjoy working with because he probably asks questions that nobody had ever thought of.’”
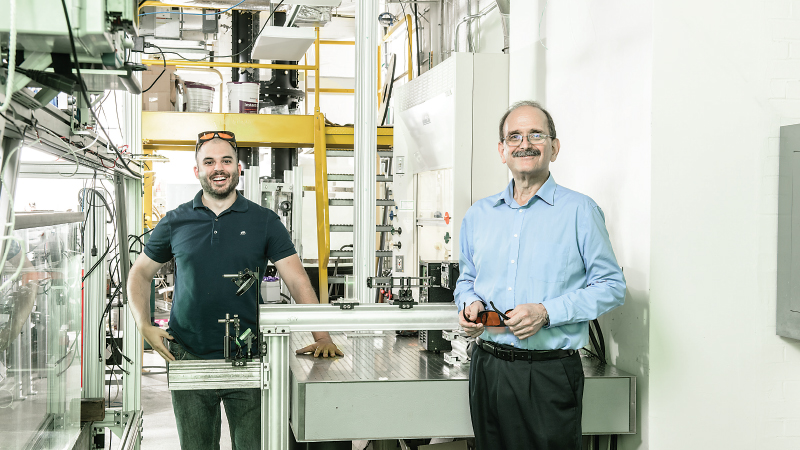
Joe Katz, 62, is a native of Tel Aviv and a veteran of the Israeli army. He has spent nearly 28 years at Hopkins studying fluid mechanics, testing flows within turbines, propellers, and parts of jet engines for government agencies and industry, becoming one of the world’s top authorities on pumps in the process. When it came time to choose the engineering lead for the project, Katz was the obvious choice: After all, what is the heart but a complex pump?
With his receding hairline and bushy mustache, he’s a dead ringer for Bill Macy, the actor who played Bea Arthur’s husband on Maude. But Katz is way smarter.
“I’ve met a lot of intelligent people, but he’s one of a kind,” says Biasetti. “He drains your energy, your entire body. He never stops. You give him a problem and he keeps going until he either hits the wall or finds a possible solution. The conversation can go on for hours and hours. He goes on thinking and thinking until he finds something that satisfies him, and you’re there trying to keep up. It’s painful, but it’s a beautiful thing talking to him.”
In the fall of 2013, Katz knew nothing about the cardiovascular system. So he set out on a journey to gather as much information as he could, picking the brains of colleagues in engineering, and meeting with cardiologists at the hospital. He sat in on open-heart surgeries and spoke with patients who use heart-assist devices, the “bridge” therapy that helps keep patients alive while they wait for a transplant heart. Dick Cheney was hooked up to one briefly in 2010, while waiting for his own transplant. As Katz discovered, the devices, called left-ventricle assist devices, or LVADs, are awkward affairs. They require bulky external power sources and infection is common where tubes enter the body. Even cardiologists aren’t fans.
“They are crude devices,” admits Cameron. “Many are kind of big, noisy, ugly things. If Apple were designing an artificial heart or an LVAD, they would look a lot different.”
Most significantly, they tend to cause thrombosis when blood clots form in the pump as well as the rupture of red blood cells, thanks to the device’s manmade materials and the rapid speeds at which the pumps must run. These failings result in strokes and other complications—big problems in artificial hearts, too.
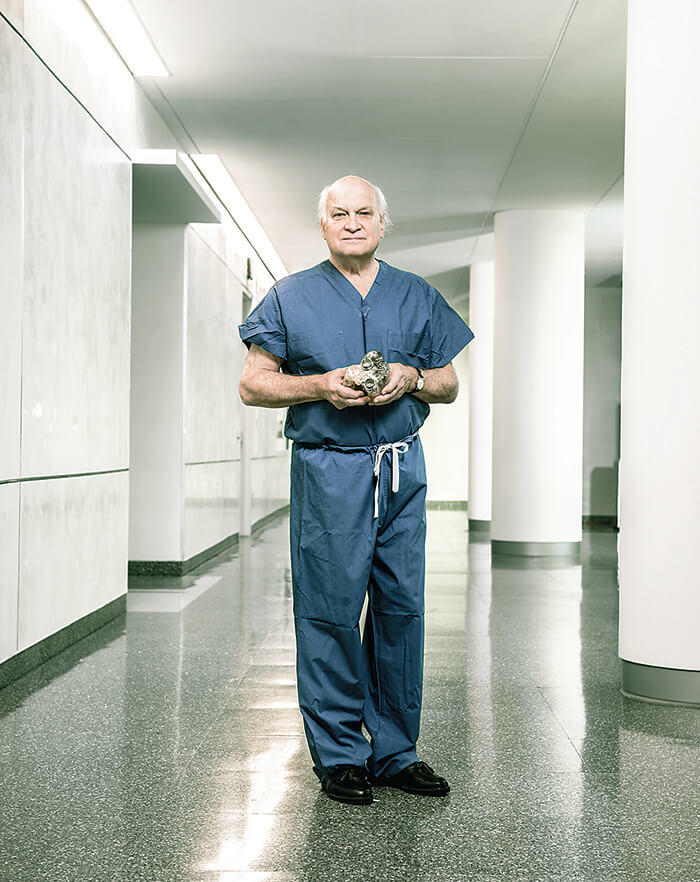
Dr. Duke Cameron, Johns Hopkins’ chief of cardiac surgery and leader of the Hopkins Heart Initiative.
So Katz realized his first order of business was to discover a way for the Hopkins Heart not to damage the blood. He and Biasetti teamed up with radiologist Assaf Gilad and hematologist Thomas Kickler, an expert in coagulation, to figure out a way to adapt the tools Katz had been using to analyze pumps for submarines and jet engines to something a fraction the size—which is exactly what Biasetti has done with his experiment. The plan was for researchers to replace the vial of plasma with a transparent LVAD so they would be able to observe blood as it flows through it and witness, on a cellular level, where the damage is occurring within. It’s basic research that the heart-assist pump manufacturers have not yet been able to perform.
For now, these experiments are being funded in part by $1 million raised so far in private donations—sourced from Cameron’s appreciative patients and some alumni from the School of Engineering. From this pot, the university has handed out “seed grants” to other Hopkins researchers, who are working on everything from attempting to grow heart muscles from stem cells to running computer simulations of various potential pump designs.
“If Apple were designing an artificial heart, they would look a lot different.”
But the Hopkins team knows they’re already playing catch-up. Similar programs at Penn State University, Yale University, the University of Louisiana at Lafayette, and the Texas Heart Institute in Houston, among others, have been at it for years, with varying degrees of success. In private industry, the most sophisticated on the market is Carmat, a French company that has already implanted three permanent artificial hearts derived from man-made materials and heart tissue from a cow. Its first two patients didn’t live longer than nine months. The company says its third patient, who received a new heart in April, returned home from the hospital in September.
Still, Katz says all of these devices are basically variations of the same, improved, but not radically different from what DeVries implanted in Barney Clark so many years ago. “The [Carmat heart] is not a breakthrough compared to what came before,” he says. “I’m not trying to downplay their efforts; in many ways, it’s the leading device in the world and until somebody like me comes up with a better product, this is it. But if you look at the overall device, it is not fundamentally different than where we were 10, 15 years ago. I’m talking about ingenuity, new concepts, and fundamentally new ideas that will make you believe that a person could live 10 years or more with this thing inside of them.”
On the road to creating a permanent artificial heart, Tomaselli says the team will likely create many other advances in cardiovascular medicine. “Along the way, like the space program, we will develop new technologies and gain an understanding of how the cardiovascular system works, and there will be a number of spinoffs that will have an impact on public health.”
An improved LVAD could be the first such technology. The Hopkins team has applied for a $2 million grant from the National Institutes of Health to further the work, and has inked a deal to collaborate on research with at least one LVAD manufacturer.
But money needs to be raised first. A lot of money. Cameron says that while the university could seek a commercial partner or investment group, he’d much prefer the project be funded by philanthropy and grants so Hopkins can keep its autonomy. “Look, there are people who write checks for $100 million these days, and we only need one of those,” he says. “What we’d like is a humanitarian, not an investor. Somebody who really wants to see lives saved.”
Potential donors not only need to buy into the idea, but so do researchers at the university. Until more funds come in, Biasetti is the initiative’s only full-time employee; faculty members are basically volunteering their time to help out.
“Kennedy threw down the gauntlet, but there were a lot of people who had to be sold on the idea,” says Cameron, who, after one early brainstorming session gave everyone in the room a copy of Marketing the Moon: The Selling of the Apollo Lunar Program, the 2014 account of one of the best public relations/marketing campaigns in U.S. history. “It’s not enough for us to be excited about it, we have to instill the excitement in everybody else.”
And like the space race between the United States and the former Soviet Union, there’s a lot of pride at stake for Johns Hopkins researchers. “Oh, it’s a race. Absolutely,” says Cameron. “But it’s not a race that will only have one winner. The winners are the patients who get the device. Whether we cross the finish line first or sixth doesn’t matter as long as something comes of this that improves lives. In the end, that’s what matters.”