Partner Content
“While lupus patients often feel very ill, for many the disease is invisible. Patients find themselves having to explain to loved ones or coworkers why they struggle, and often feel misunderstood.”
Ashira D. Blazer, MD, MSCI became interested in rheumatology while in medical school when, as she was studying for her musculoskeletal block exam, she received a call from her cousin who had been unwell. Listening to her cousin’s symptoms with her textbook open, Blazer realized her complaints matched those of lupus. Her cousin was able to get a formal diagnosis and treatment plan and, for Blazer, studying lupus has become a way to marry her scientific interests with her sense of caring for the community. Here she talks to us about the signs of lupus, new treatments, and creating equity around care for the condition.
What are the classic signs of Lupus?
With lupus, the immune system, which should protect you against viruses and bacteria, becomes active against your own healthy tissues. Most commonly patients develop rashes, sun sensitivity, joint pain, hair loss, or severe fatigue. Lupus can also affect the internal organs such as the heart, brain, or most notably and commonly, the kidneys.
Who is at greater risk of developing Lupus?
African American women are at the highest risk both for developing lupus and for having more severe manifestations of it. Additionally, factors such as infections, sun and other environmental exposures, stress, and processed foods have all been shown to increase risk.
How can Lupus impact daily life?
One of the most debilitating symptoms of lupus is overwhelming fatigue. Patients report having difficulty getting out of bed in the morning, let alone taking care of their daily tasks or work obligations. Patients may also struggle with forgetfulness, or joint pain that prevents them from doing everyday things. While lupus patients often feel very ill, for many the disease is invisible. Patients find themselves having to explain to loved ones or coworkers why they struggle, and often feel misunderstood. For those who have rashes or hair loss, lupus can be disfiguring.
What research is currently underway regarding new treatments?
Traditionally, lupus has been treated with immune suppressing medications or steroids. While these medications can decrease inflammation, they also carry unacceptable side effects. In fact, many of the most serious outcomes in lupus, like severe infections or heart disease, result from high doses of steroids for extended periods of time. Newer therapies for lupus are aimed at impacting the disease course while preventing patients from needing high doses of steroids. The University of Maryland is at the forefront of this discovery, as we have several ongoing clinical trials.
How would you like to see the discussion around Lupus change and why?
Lupus most frequently effects women of color, who also face socioeconomic disadvantage and discrimination. These social factors directly influence health outcomes and access to effective therapies; however, we rarely think about how to address these problems clinically. Too often poorer outcomes among our patients of color are blamed on inherent biologic differences. I would like to see more emphasis being placed on getting patients an early diagnosis and management. There should be a standard of care that we strive for, and we should work to ensure that patients of all backgrounds are able to achieve and maintain that standard.
What is the biggest myth about rheumatic conditions?
The biggest myth is that the conditions don’t get better, and they will undoubtedly change the entire trajectory of one’s life. There can be a big stigma particularly among women looking to start families. Lupus patients who achieve low disease activity can enjoy the same extended lifetimes as people who don’t have lupus. They can work, get pregnant and start families, and can live fulfilling lives. With stable and continuous therapy, lupus and other rheumatic diseases can be well managed.
What do you enjoy most about this field?
I take care of patients who have been looking for a diagnosis sometimes for years on end. I love to offer the first sign of an explanation to my patients. Hearing someone validate how they’ve been feeling gives them a huge sense of relief. We then outline a plan to help them get their lives back. Since I treat mostly young women of color who have lupus, I allow these incredible and driven people to get a sense of normalcy.
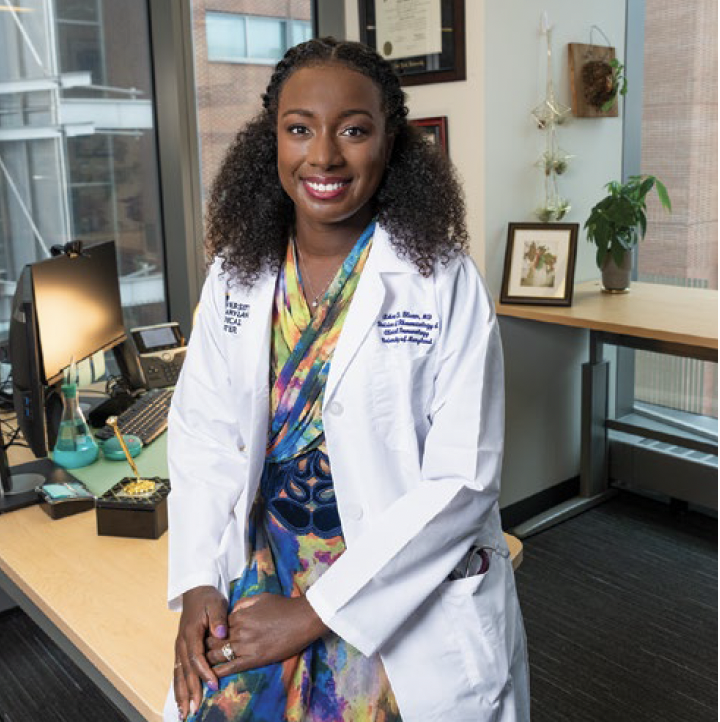
MEET THE EXPERT:
Ashira D. Blazer, MD, MSCI
Assistant Professor of Medicine,
University of Maryland School of Medicine
Rheumatologist
Locations:
Baltimore City

